RNY GASTRIC BYPASS SURGERY
Roux-en-Y gastric bypass is considered the gold standard in treating morbid obesity
Laparoscopic Gastric Bypass (RYGB) – Also known as Full Bypass – Weight Loss Surgery in Tijuana, Mexico
Gastric bypass surgery is a combined restrictive-malabsorptive procedure that makes the stomach smaller and causes food to bypass part of the small intestine. You will feel full more quickly than when your stomach was its original size. This reduces the amount of food you can eat at one time. Bypassing part of the intestine reduces how much food and nutrients are absorbed. This leads to weight loss.
One type of gastric bypass surgery is a Roux-en-Y (RNY) gastric bypass, is the most common form of weight loss surgery performed in the United States today.
PROS:
-
The best option for patients with GERD (resolves completely or significantly decreases in 95% of patients immediately post-op), strong heartburn, esophagitis, Barrett`s esophagus.
-
Stronger restriction compared to Mini bypass due to a smaller (tighter) anastomosis in RNY bypass.
-
Great option for patients with higher BMI over 50 as a first time surgery or as a second step after gastric sleeve to promote further weight loss (in case of weight regain or insufficient weight loss after the sleeve).
-
Preferred option for patients with Type 1 diabetes (insulin dosage decreases significantly) and Type 2 diabetes (resolves completely for most patients) due to malabsorption.
CONS:
-
More complicated procedure compared to Mini bypass or gastric sleeve with potentially higher complication risk (2 intestinal anastomoses in RNY bypass vs 1 anastomosis in Mini bypass).
-
Higher risk of developing marginal stomach ulcers (ulcers at the site of the stomach and intestinal connections) compared to gastric sleeve.
-
In RNY bypass the lower stomach sphincter is no longer intact, and depending on how well the stoma area scars, may result in stronger or reduced feeling of restriction. Learn more at Restriction after gastric sleeve vs restriction after Mini or RNY bypass.
WHY WAS THE RNY BYPASS DEVELOPED?
Metabolic surgery starts its history from 1954 when the first malabsorptive procedure was introduced by Dr.Kremer to treat dyslipidemia. As morbid obesity became of serious concern worldwide, this procedure was further improved and the first laparoscopic traditional gastric bypass (RNY) was performed in 1994 by Dr. Alan Wittgrove. The main purpose of this surgery was to treat morbid obesity in high BMI patients, since then it became acceptable among low BMI patients (BMI < 35) with certain comorbidities like diabetes or GERD, or as a revisional procedure. RNY bypass surgery is a both restrictive and malabsorptive procedure. This means that it reduces the stomach to about the size of an egg (1 – 2 oz), restricting the amount you can eat; it also reduces absorption of food by bypassing up to 5-8 feet of the small intestine (more is bypassed in higher BMI, less in BMI under 35). Studies show that RNY bypass leads to more weight loss compared to gastric sleeve and weight loss results last longer.
To learn about how RNY Bypass compares to other weight loss surgeries, pros and cons of each procedure, please go to Compare Bariatric Surgeries.
SURGICAL METHOD
-
Inflate the abdomen with CO2 gas to create sufficient space around the stomach and intestines. The abdomen will be deflated at the end of surgery, however some gas residue will remain and cause pain and discomfort (on the left side and left shoulder in particular). Walking as much as you can after surgery will help to reduce pain and remove gas much faster. Learn more at Pain. Left side stabbing pain or left shoulder pain, early recovery stage.
- Perform an endoscopy to check on the stomach condition. Learn more about the pre-op and post-op endoscopy here >>
- If the liver is large, a special instrument called liver separator will be inserted to keep the liver in an uplifted position throughout surgery to allow access to the stomach.
- Hiatus (an opening in the diaphragm where the esophagus connects to the stomach) will be examined to check if hiatal hernia is present. If a hiatal hernia is diagnosed and it is large, it will be repaired during surgery by suturing the opening in the diaphragm. The stomach will be pulled into its correct natural position and if need be anchored by a so-called anchor stitch (it is important to stress that there is no guarantee a hiatal hernia will not develop again in the future).
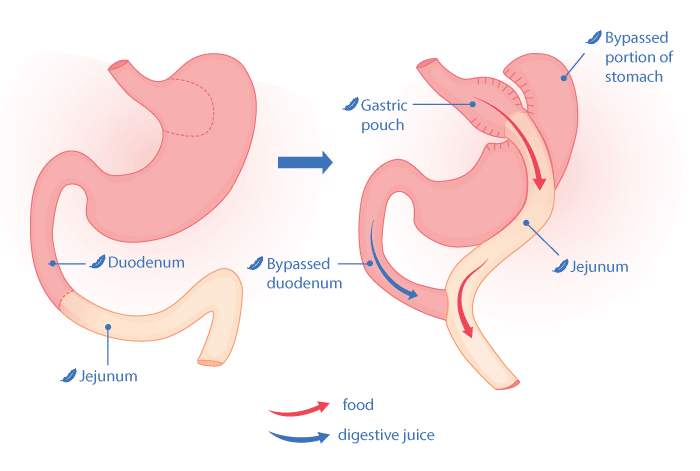
- With the help of a laparoscopic stapler, the surgeon separates a tube-shaped chamber from the stomach at the base of the esophagus, it will be connected to the small intestine, this will form the first anastomosis (connection between the stomach pouch and the small intestine). The remaining part of the stomach is no longer attached to the esophagus and will no longer receive food. It does remain in your body in its original position and continues producing stomach acid that flows into the small intestine and helps to digest food. The volume of your new stomach pouch is much smaller, about 1 to 2 oz which results in restrictive feeling and smaller food portions. The pouch has the shape of a small tube.
- The surgeon will create a Y-shaped anatomy of the digestive tract formed by the stomach pouch and two parts of the small intestine: the biliary limb and the Roux limb (this is where the name of Roux-en-Y comes from). The doctor will measure out about 100 to 150 cm (3 to 5 feet) of the small intestine called duodenum (also known as biliary limb) that follows the larger part of the stomach that has been separated (see the image above). Food will no longer pass through the duodenum (biliary limb) where most of the calories and nutrients are absorbed, this produces a malabsorptive effect and results in more drastic weight loss. But the stomach juices and liver enzymes (bile fluids) that help to digest food will pass through and reach food further down. The surgeon will also measure out another 70 to 120 cm (2 to 4 feets) of the small intestine called jejunum (or Roux limb) that will follow the new small stomach pouch. Food will be passing through this portion of the small intestine. Finally, the biliary limb and the Roux limb will be stapled together creating a second intestinal connection – duodenojejunal anastomosis. At this point food passes through a so-called common channel, meaning that digestive enzymes from duodenum and food from jejunum will be united in the remaining portion of the small intestine, this is called a common channel.
- Since quite a lot of intestinal movement is involved to perform a bypass, the small intestine must be separated from the visceral fat tissue that surrounds our internal organs. This is why a good pre-op diet is so important for any type of bypass surgery: the better the diet, the less internal fat tissue (visceral fat) surrounds the intestines, the less cutting is needed, which results in less blood loss, less risks and faster recovery.
- In certain cases the surgeon removes the Fundus portion of the stomach that is located in the upper part of the stomach. This may be necessary in case of a higher complication risk, if stomach polyps are diagnosed in the Fundus, or due to the scar tissue after previous abdominal surgeries that complicate access to the stomach, due to a very large liver and other factors. Removing the fundal portion of the stomach has its pros and cons: it makes a bypass surgery slightly easier for the surgeon and reduces the risk of post-op stomach ulcers (the larger the stomach pouch, the more possibilities for ulcers to develop); some research shows that it also decreases hunger during the first months post-op by reducing production of the hormone Ghrelin that is mainly produced in the Fundus; it does however increase the risk of the post-op bleeding (the more cutting is done, the more blood vessels may bleed).
- A second endoscopy is performed to check for potential staple or suturing line disruptions, bleedings, etc.
- Drain tube will be placed (it is removed on the day of the hospital discharge).
- All the incisions are closed with 100% dissolvable stitches except for one incision that is sutured internally with non dissolvable material and externally with dissolvable suturing. This particular incision that is normally located toward the right side of the abdomen above the belly button is closed in this special way in order to prevent incisional hernia, since this incision is used more than others during surgery and thus is more traumatized. More surgical instruments are inserted and removed through this incision, if a portion of the stomach is removed, it is pulled through this incision also. Pain in this incision is expected to be a little stronger and longer-lasting compared to others. Fibrous tissue that feels like a ball or a lump when pressing on the area around that incision is normal during the first few months post-op and will reduce with time.
For better understanding of the anatomy of RNY bypass, we invite you to watch the video below, courtesy of Ethicon, our trusted provider of bariatric titanium staples and other surgical instruments.
HOW YOU LOSE WEIGHT?
Restriction:
RNY gastric bypass restricts the amount of food you can eat by creating a small stomach pouch, for many patients it also reduces hunger (at least during the first few months post-op);
Malabsorption:
RNY gastric bypass reduces the number of calories your body will absorb from the food you consume due to a large portion of the small intestine being bypassed.
WEIGHT LOSS IS RAPID:
Statistics show that most RNY bypass patients lose more than half or even all of the excess weight over a short term (1 to 1.5 years) and do not regain over a longer period of time compared to gastric sleeve surgery, however results vary. Factors to consider include the initial BMI (starting weight at the time of the pre-op diet and on the surgery day, the lower the BMI the slower is the weight loss but the more chances to lose all of the excess weight), age (pre-menopause or postmenopause), previous weight loss surgeries, thyroid function, adherence to the low-carb protein diet for the rest of your life, physical activity, water intake, gender, amount of muscle tissue (the more muscles the more calories our body burns even in the state of resting), hours of sleep, level of stress, etc.
As with all bariatric surgery procedures, weight regain does occur (most of the time due to the patients` incomplete adherence to the post-operatory guidance or slow return to the old eating habits), but most patients are able to keep at least half of the excess weight off over a long term due to the malabsorptive effect of the RNY bypass.
Success is higher among people who have realistic expectations about how much weight will be lost, keep appointments with the medical team, follow the recommended diet guidelines, are physically active and work either alone or with a therapist on their emotional and mental health and change their relationship with food as well as learn how to cope with stress without relying on food as the main source of pleasure. Our bariatric nutritionists and therapists are available to consult and support you all along your weight loss process in order for you to fully benefit from the procedure and reach your desired weight.
SURGERY TIME
On average, Dr. Cynthia Hernandez and Dr. Francisco Zavalza take 1 hour to perform RNY gastric bypass surgery (the time may increase in case of a revisional procedure or if a patient has a lot of scar tissue after previous abdominal surgeries). Then the patient is taken from the Operation Room to the Recovery Area where under close observation by nurses and doctors the patient wakes up from the anesthesia, all vital signals and oxygen levels are monitored. After about 1 -1.5 hours in the recovery area, the patient is taken back to their hospital room, where if accompanied by a family member he is reunited with their companion for the rest of their hospital stay.
If a patient travels alone, our on-site facilitating team that is present at the hospital 24/7 will be happy to inform the family members who stayed at home about the outcome of the procedure and the patient`s recovery status (of course if the patient requests such updates prior to surgery).
HOSPITAL AND HOTEL STAY
Two days and two nights are required at the hospital for the RNY gastric bypass in Tijuana, Mexico.
(Please visit What to Expect in Tijuana and NEWCITY Hospital or CIBA Surgical Center for more details).
Two nights at the hotel are recommended, but three nights are included in the surgery package to allow for additional recovery if needed.
Plan your trip for a RNY bypass surgery in Tijuana this way:
Day 2. Surgery, hospital stay.
Day 3. Hospital stay.
Day 4. Discharge, hotel stay.
Day 5. Departure or additional hotel stay (this night is optional).
Day 6. Departure.
RECOVERY TIME
- For a sedentary type of work – a minimum of 10 days off is recommended.
- If your job requires more strenuous physical activity and lifting over 15 pounds, we recommend at least 2-3 weeks off.
- The weight lifting restrictions are: up to 15 pounds for 2-3 weeks post-op, and up to 35 pounds for another 2-3 weeks. After 6 weeks you may go back to normal weight lifting but gradually.
- For jobs that require strenuous physical activities and long working hours such as nurses, as an example, we recommend 4 weeks off.
- Keep in mind that you will feel very weak and lack energy, and get easily tired during the first 4 to 8 weeks post-op due to a low-calorie diet and dehydration. So, it may be difficult to concentrate on work (mental or physical) during this time until your body adjusts and your diet progresses to the point where you can tolerate a greater variety of foods and more calories. Usually energy levels return after 8 weeks post-op.
Short Term Disability or FMLA paperwork:
Our medical team will gladly complete the required forms for your employer. If you need a simple doctor`s note to take time off or a return to the work release note, please request one with your patient coordinator.
Send the forms (STD or FMLA) to your patient coordinator via email or fax them to 855-457-1400. Please be sure to complete the portion of the form that is non-medical related. Our medical team will complete only the portion of the form that is required to be completed by the attending physician. Usually, the top portion of any form asks for the patient to enter their personal and job-related information.
When you send us the form, please answer the following questions along with it:
1. The first day off work;
2. The day you plan on returning to work;
3. Will you need any work restrictions for a certain period of time after you return to work, such as no heavy lifting, light duty, frequent breaks, etc.? If yes, for how long, or will you need a release to full duty?
Our medical team takes 7 business days to process the forms; please send them, taking into consideration the processing times.
BENEFITS OF RNY GASTRIC BYPASS
- More dramatic weight loss compared to only restrictive bariatric surgeries (such as gastric sleeve).
- Statistically longer lasting weight loss results (less percentage of patients regain the weight).
- Works by both restriction and malabsorption.
- Substantial improvement in many health problems related to morbid obesity, such as (but not limited to):
✓ Lower risk of heart attack and other serious cardiovascular issues
WHAT TO EXPECT AFTER RNY BYPASS SURGERY IN MEXICO
- Recovery, pain, and complications are very similar to any other type of bariatric weight loss surgery.
- Pain is usually caused by the gas residue in the abdominal cave and walking helps to get rid of it faster. By the 3rd day post-op when the patient is discharged from the hospital, pain is easily manageable by non-opioid painkillers.
- In order to prevent blood clots, blood clot symptoms, and to promote healing, our medical team will have you up and moving as soon as possible following surgery. Special compression stockings will be used on your legs to help with blood clot prevention. Extra blood thinners may be prescribed upon hospital discharge, this is determined by our internal medicine doctors for each patient individually. Learn more about factors that increase blood clot risks here.
- Because the surgery makes your stomach smaller, you will get full more quickly when you eat. Food also may empty into the small intestine too quickly and lead to dumping syndrome. This can cause diarrhea and make you feel faint, shaky, and nauseous. It also can make it hard for your body to get enough nutrition. The same post-op diet is recommended for all surgery types. It is important to follow it without skipping any stages and without rushing, this will allow for a smooth recovery.
- During the first month after surgery, your stomach can only handle small amounts of soft foods and liquids while you are healing. Bit by bit, you will be able to add solid foods back into your diet. And after approximately one to two months you will come back to normal solid food intake. However, you will be asked to follow a new diet that will include more protein, vegetables and fruit for the rest of your life. Your stomach is much smaller and there is no room for junk food (you need to maximize nutrients from every bite you eat).
- It is important to keep sipping water throughout the day to avoid dehydration. Learn more about post-op dehydration (IV hydration)
- You may notice that your bowel movements are not regular right after your surgery. This is common, and if the condition lasts for more than 4 or 5 days you may need to use a light laxative, however, do consult your doctor before taking any additional medication. Learn more about post-op constipation.
- You must chew food very thoroughly and learn to stop eating when you feel full. This can take some time to get used to. If you do not chew your food well or do not stop eating soon enough, you may feel discomfort or nausea and may sometimes vomit.
- If you drink a lot of high-calorie liquids such as soda, fruit juice, milk, frappuccinos, etc., weight loss will slow down, stop and eventually you will start regaining the weight. The importance of food texture (solid foods vs liquids) in any type of bypass surgeries is explained in Restriction after gastric sleeve vs restriction after Mini or RNY bypass.
- If you continually overeat, the new stomach pouch and pouch opening (stoma) will stretch. If the stoma stretches, you will not benefit from your surgery and its restrictive effect will be lost.
- In RNY bypass, the part of the intestine where many minerals and vitamins are most easily absorbed is bypassed. Because of this, you may have a deficiency in iron, calcium, magnesium, or vitamins. This can lead to long-term problems, such as osteoporosis. To prevent vitamin and mineral deficiencies, our nutritionists will work with you on your vitamin intake and analyse your post-op lab work results. Taking vitamins post-op is highly recommended after RNY bypass for the rest of your life.
- Post-op lab work is recommended for all surgery types at 3-, 6-, 12, and 24-months post-op. Learn more at Blood work post-op.
- It is important to avoid heavy lifting: no more than 15-20 lb for the first 2-3 weeks, then no more than 35 lb for another 2-3 weeks. After 6 weeks it is safe to resume regular weight lifting but gradually.
- Light exercising is recommended after surgery as soon as you gain enough energy: walking, walking up the hill, elliptical, very light weights. Strenuous exercising is not recommended until 2 months post-op. Once your diet progresses to the stage where you can tolerate a greater variety of foods and your caloric intake increases, it is beneficial to add regular exercising to boost further weight loss.
RISK OF RNY GASTRIC BYPASS SURGERY
It is important to understand that all types of bariatric surgery carry certain risks. Most of the serious complications happen within the first 24 to 48 hours post-op, while the patient is still at the hospital, and our medical team takes care of the issue immediately. Extra expenses associated with a surgery complication that is not caused by a pre-existing condition are covered for our patients. Learn more about our Medical Complication Insurance that is included in each surgery package automatically. Our surgery complication rate is between 0.001 and 2%, depending on the type of complication.
It is not always possible to collect the correct statistical data as not all our patients report on how their recovery progresses and many eventually stop regular communication as they approach their goal weight. These are the numbers based on our observations among our own patients since 2014 (the statistics based on the data collected worldwide may be different):
Incisional hernia – 3 patients
Postoperative Bleeding – 1.5 % of patients
Gastrointestinal leak – 3 patients (1 after a gastric sleeve, 2 after a revision from sleeve to RNY bypass)
Marginal ulcers – 1.5 – 2% of bypass patients
Blood clots – 1 or 2 patients had pulmonary embolism, at least 3 or 4 had DVT (deep vein thrombosis)
Stenosis or stricture – less than 1% for all surgery types
Wound sepsis – less than 0.5% of patients
Bowel obstruction – less than 1% of bypass patients
Esophageal issues – 1 patient
Severe malnutrition – 1 or 2 patients
Death rate – 0 %, 0 patients
Some of the above are minor and easily treated, while others can be more serious. Such surgery consequences as phlebitis (temporary vein inflammation due to an IV infiltration) or acid reflux as a side-effect of the gastric sleeve are not considered acute surgery complications.
LOWER YOUR RNY GASTRIC BYPASS SURGERY RISKS
Before having any type of weight loss surgery, you can limit post-op side effects and complications by following these steps:
- Be completely honest in your medical questionnaire and when speaking to the medical team before surgery, do not hide any health conditions.
- Lower your BMI and shrink the fatty liver by strictly following the pre-op protein diet.
- Quit smoking cigarettes and marijuana, drinking alcohol, coffee and sugary/carbonated beverages, any type of street drugs.
- Exercise regularly (even if it is only walking)
- Stop (or continue) certain medications before surgery according to our medical team`s instructions (antacids, NSAIDs, hormonal medications, etc.)
- Start taking vitamins pre-op
HOW DO I KNOW IF RNY BYPASS SURGERY IS RIGHT FOR ME?
Even though RNY bypass is a more serious and complicated procedure than Mini bypass or gastric sleeve, there are a few significant reasons why this procedure may be your best option.
Due to the Y-shaped anatomy of this procedure, the stomach acid is diverted from the stomach pouch, thus fixing or significantly reducing acid reflux (or GERD).
- For patients with a large hiatal hernia, RNY bypass is a much better option rather than the gastric sleeve.
- Patients with high BMI > 50 rarely achieve their goal weight with gastric sleeves only. Such patients may choose RNY to bypass as their initial procedure or as the second step after the sleeve to promote more drastic weight loss results.
