WHY CONSIDER GALLBLADDER REMOVAL WITH
WEIGHT LOSS SURGERY?
It is difficult enough to decide to have a weight loss surgery. It can be even more difficult to decide to have an entire body organ to be removed. Dr.Zavalza does not encourage every bariatric patient to remove gallbladder, however we strongly advise that you seriously consider such procedure and make your own research, especially if you are in a high risk group, as you will learn further.
In this article:
What is the gallbladder?
What are gallstones?
Who is at high risk of developing gallstones?
What are the symptoms of gallstones?
How are gallstones diagnosed?
What are the complications of untreated gallstones?
What happens during gallbladder removal surgery?
What is the cost of gallbladder removal in Mexico?
What are the side-effects of living without a gallbladder?
How can gallstones be prevented?
What is the gallbladder?
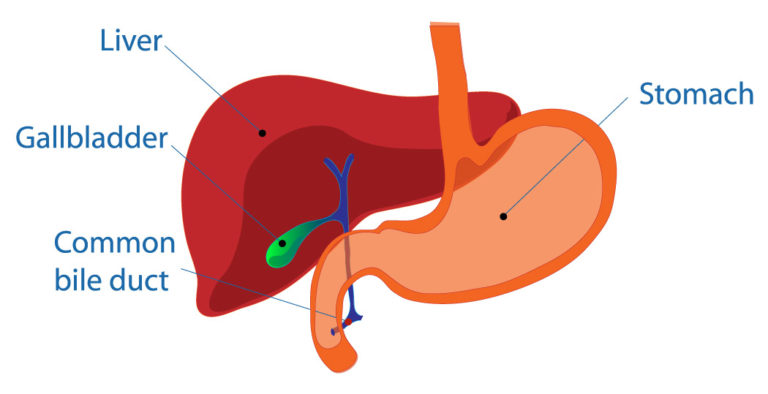
Before discussing the issue of gallbladder stones, we need to understand what is the gallbladder and its role. Gallbladder is a small pear-shaped organ that sits on the right side of our body under the liver and connects on one end to the liver, and on the other end to the small intestine. It serves as a storage unit for bile, a yellowish-brown liquid that helps with food digestion. The liver produces about a quart of bile every day, and the gallbladder holds an ounce of it at any time, slowly dripping it into the small intestine.
Bile, also called gall, among other substances consists of acids, salts and cholesterol; the exact composition varies from person to person and depends on different factors such as diet for example. It`s main role is to helpour body break down fatty foods and absorb nutrients from them.

What are gallstones?
Gallstones form when cholesterol, the main ingredient dissolved in bile, comes out of the solution and clumps into pebbles (just like a jar of peanut butter eventually separates into solid and liquid parts). It is believed that the process starts with small crystals that form in bile, and cholesterol clumps build up on top of those, like an oyster pearl.
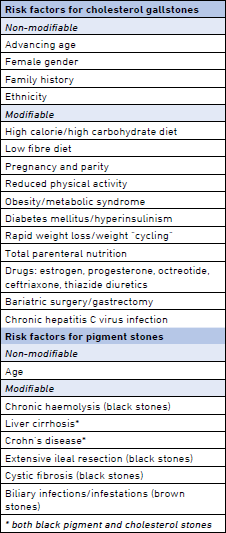
According to NIDDK there are 2 main types of gallbladder stones: cholesterol stones (yellow-green, made of hardened cholesterol, the most common type) and pigment stones (darker in color, composed of bilirubin, a side-product of natural red blood cells breakdown process). Gallstones vary in size from a grain of sand to a golf ball, however, symptoms do not depend on the size or number of gallstones. A person who has one gallstone (small or big) could experience the same symptoms as a person with many larger or smaller gallstones. Gallstones can be present in the gallbladder itself, which is called cholelithiasis; or in the bile duct (a small tube that delivers bile into the small intestine), which is called choledocholithiasis.
WHO IS AT HIGH RISK OF DEVELOPING GALLSTONES?
According to The World Gastroenterology Organization gallstone disease is a growing global burden (https://www.worldgastroenterology.org/publications/e-wgn/e-wgn-expertpoint-of-view-articles-collection/the-growing-global-burden-of-gallstonedisease). Up to 20% of women and 10% of men in the US develop gallstones by the age of 60, and in the recent decade more and more younger people have been affected, including teenagers.
The key risk factors are the following:
• Obesity is a major risk factor for cholesterol gallbladder disease (GD), which includes gallstones and other gallbladder issues. Researchers have found that overweight people have higher levels of cholesterol in their bile, which can cause gallstones; they also often have larger gallbladders that do not function (empty itself) properly. Some studies have shown that people who carry large amounts of fat around their waist may be more likely to develop gallstones than those who carry fat around their hips and thighs. Women are more likely to develop gallstones due to sex hormones: estrogen increases the amount of cholesterol in the bile, while progesterone slows the emptying of the gallbladder. These risks increase with pregnancy or even oral contraceptives, as they alter hormone levels.
• Rapid weight loss
Bariatric surgery patients are prime candidates for developing gallstones. Weight loss at a rate of more than 2 pounds per week is considered rapid, and most weight loss surgery (WLS) patients lose a significant amount of weight in the first 3 to 6 months post-op. The type of surgery does not matter, as it is weight loss itself that causes gallstones: when we do not eat for a long period of time, or when we lose weight fast our liver releases more cholesterol into the bile, also fast weight loss causes slower gallbladder emptying, thus promoting gallstones formation.
International Journal of Obesity mentions a 1-year study research on patients that followed a very low calorie diet compare to just low calorie diet. The results showed that the risk of gallstones requiring hospitalization or gallbladder removal was 3 times greater among patients who followed a very lowcalorie diet. Also, if you had so-called silent gallstones (that never bothered you before WLS), you are more likely to develop gallstone symptoms after bariatric surgery. Weight cycling, or losing and regaining weight repeatedly, may also lead to gallstones. The more weight you lose and regain during a cycle, the greater your chances of developing gallstones.
• Diabetes Mellitus
People with diabetes generally have high levels of fatty acids, called triglycerides, which increase the risk of gallstones.
• Metabolic syndrome (MS)
The association between GD and obesity is now recognized as part of the MS, which includes central obesity, high triglyceride and low HDL-cholesterol levels, glucose intolerance, and hypertension. Hepatic insulin resistance stimulates cholesterol secretion into bile and impairs bile acid synthesis, favoring gallstone formation. Hepatic insulin resistance is associated with GD even in non-diabetic, non-obese individuals.
• Non-alcoholic fatty liver disease (enlarged liver)
• High triglyceride levels
• Low HDL cholesterol
Drugs that lower cholesterol in blood can actually increase the amount of cholesterol secreted in bile, which, in turn, increases the risk of gallstones.
• “Western-type” Diet
Chronic overnutrition with refined carbohydrates and reduced intake of dietary fiber might account for the increased cholesterol gallstone prevalence.
• Hereditary factor
People with a family history of gallstones have a higher risk
• Race
American Indians have genes that raise the amount of cholesterol in their bile, and have the highest rate of gallstones in the United States. Mexican Americans are also at higher risk of developing gallstones.
• Decreased physical activity
• Liver cirrhosis and chronic Hepatitis C
• Crohn’s disease
WHAT ARE THE SYMPTOMS OF GALLSTONES?
For a while most gallstones do not cause any symptoms, so-called silent stones. But as soon as they start moving and obstruct the bile duct (a small hose that delivers bile into the small intestine) they cause gallbladder inflammation and “attacks” begin to occur.
- Abdominal pain
It is important to understand the pattern of pain: it usually starts on the right side of the upper abdomen, just under the rib cage, and can radiate to the right shoulder, between the shoulder blades, or to the center of the abdomen. It usually occurs within two hours after a meal that contains fat (a pattern of fatty food intolerance) and can last anywhere between an hour and several hours. If the pain doesn`t go away for more than a few hours, it can indicate a more severe gallbladder issue that requires hospitalization. If pain starts while you are still eating or immediately after eating (within 15 minutes), it might indicate a different issue, that is not connected to the gallbladder.
- Painkillers don`t help
If after taking a painkiller (Tylenol or Ibuprofen for instance) pain does not go away, it can also indicate a gallbladder issue. If changing body position, or after a bowel movement, or passing gas you feel slight relief, it is another indication of a gallbladder problem.
- Jaundice
Jaundice is a symptom when a person develops yellowish skin and the whites of the eyes. The gallbladder releases bile into the small intestine through small tubes, called ducts (cystic and bile ducts), when gallbladder stones start moving through those ducts, they get obstructed, and bile gets accumulated in the gallbladder. This in turn causes higher levels of a yellowish substance called bilirubin.
- Nausea and vomiting
This symptom is not as common as abdominal pain and is often mistaken for heartburn, or acid reflux (especially after Weight Loss Surgery), or upset stomach. However, if nausea and/or vomiting occurs repeatedly after eating, it may indicate a gallbladder issue.
- Pancreatitis
If you develop pancreatitis, an inflammation of the pancreas, you should be checked for gallstones. This is because the gallbladder and pancreas share a bile drainage duct, so an obstructing gallstone can prevent the flow of pancreatic enzymes. Pancreatitis symptoms can include abdominal pain, nausea and vomiting, a rapid pulse, and a fever.
- Dark urine & Clay-colored stool
Bile salts when released in the small intestine give stools brown color. When bile is not released as a result of blockage by gallstones, the stools will have pale clay-like color. If this happens once in a while, it may not be a cause for concern. If it occurs frequently, you may have a serious illness, like gallbladder disease.
- Fever—even a low-grade fever—or chills.
- Abdominal bloating. Indigestion. Belching or gas.
See a doctor right away if you have these symptoms:
• Pain that lasts more than several hours
• Jaundice and clay-colored stool
• Fever, sweats and chills
• Nausea and vomiting
These symptoms may be signs of a serious infection or inflammation of the gallbladder, liver, or pancreas. Gallstone symptoms may resemble symptoms of other conditions, such as heart attack, appendicitis, ulcers, pancreatitis, hepatitis, irritable bowel syndrome, hiatal hernia, kidney stones, and gastroesophageal reflux disease, all of which should be treated by a doctor as soon as possible.
How are gallstones diagnosed?

Usually “silent gallstones” are discovered accidentally when testing for another health issues. However, if pain persists for several hours or happens again and again, your doctor may perform the following diagnostic procedures:
• Ultrasound
A diagnostic technique that uses high-frequency sound waves to create an image of the internal organs.
• Cholecystography
X-ray that shows the flow of contrast fluid through the intestines into the gallbladder.
• Blood tests
These look for signs of infection, obstruction, jaundice, and/or pancreatitis.
• Computed tomography scan (also called a CT or CAT scan)
A diagnostic imaging procedure that uses a combination of X-rays and computer technology to produce horizontal, or axial, images (often called slices) of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general X-rays.
• Magnetic resonance imaging (MRI)
MRI machines use radio waves and magnets to produce detailed images of your organs and soft tissues without X-rays. MRIs can show gallstones in the ducts of the biliary tract.
• Endoscopic retrograde cholangiopancreatography (ERCP)
ERCP combines upper gastro endoscopy and x-rays to treat problems of your bile and pancreatic ducts. ERCP helps the health care professional locate the affected bile duct and the gallstones. This test is more invasive—or involves more instruments inside your body—than other tests. Doctors use it selectively, usually to remove a gallstone that is stuck in the common bile duct.
WHAT ARE THE COMPLICATIONS OF UNTREATED GALLSTONES?
Gallstone complications can occur if your bile ducts remain blocked. Left untreated, blockages of the bile ducts or pancreatic duct can be fatal. Among the most common complications are:
- Gallbladder inflammation (called acute cholecystitis).
- Bacterial infection of the biliary tract (called Acute Cholangitis) is caused by a bacterial infection of the biliary tract in a person with biliary obstruction. It can cause severe damage to the gallbladder, bile ducts, or liver.
- Pancreatitis. Refers to inflammation of the pancreas and most commonly occurs as a complication of gallstones.
- Gangrenous Cholecystitis. This is the most common complication of cholecystitis, especially in older people, people with diabetes, or people who delay seeking treatment for their gallbladder attacks. Gangrenous cholecystitis is considered a medical emergency, requiring surgical removal of the gallbladder (a cholecystectomy) right away.
- Gallbladder perforation. If the gallbladder becomes gangrenous, a perforation (or a hole in the wall of the gallbladder) may develop resulting in a pericholecystic abscess (a collection of pus within the gallbladder). This complication is serious and life-threatening, requiring an emergent cholecystectomy.
- Cholecystoenteric Fistula. Gallstone Ileus. If a hole (perforation) forms in the gallbladder, a fistula (passage) into the small intestine may develop. If a gallstone passes through that passage, a bowel obstruction may occur (called gallstone ileus).
- Emphysematous Cholecystitis. This complication is caused by infection of the wall of the gallbladder with gas-forming bacteria. People most at risk for this gallbladder complication include those of older age and those with diabetes.
WHAT HAPPENS DURING GALLBLADDER REMOVAL SURGERY?
Gallbladder removal surgery, also called cholecystectomy, is one of the most commonly performed on adults in the US. This gallstone treatment method is the most common and effective compare to non-surgical treatments. The American Gastroenterological Association reports that 90 percent of these surgeries are performed laparoscopically, or with minimally invasive techniques, which promotes much faster recovery and lower complication risks.
During laparoscopic surgery under general anesthesia the doctor will make 3 or 4 small incisions (each incision less than 1 inch long) around the belly, insert surgical instruments that include a tiny video camera. While looking at the computer monitor, the surgeon will remove the gallbladder. Such procedure may take anywhere between 20 minutes to 2 hours depending on the condition of the gallbladder.
In the US many such procedures are performed on an outpatient basis, meaning a patient may be able to be discharged that same day.
Dr.Zavalza performs gallbladder removal either as a single procedure or as an additional procedure to the bariatric surgery of your choice, in the latter case hospitalization for 2 or 3 nights is already arranged. No additional incisions are necessary, as laparoscopic bariatric surgery already requires 3 or 4 small incisions. When a patient chooses to have a single incision gastric sleeve with gallbladder removal, one additional incision is necessary besides the main incision in the belly button and the drain tube incision on the left side of the stomach.
The recovery time for bariatric patients who choose to have gallbladder removed at the time of their WLS is no different from other patients. Most are able to go back to a sedentary type of work within 1 week.
Non-surgical gallstones treatment methods include:
• Oral medication to help dissolve stones (one of such medications, Ursodiol, can take years to actually dissolve stones completely).
• Injection into the gallbladder with a special solution to dissolve stones.
• Extracorporeal shockwave lithotripsy (ESWL). A procedure that uses shock waves to break stones up into tiny pieces that can pass through the bile ducts without causing blockages. That technology has not been shown to be helpful for patients with gallbladder disease, because gallstones are fundamentally different from kidney stones. A common issue for non-surgical treatment methods is: once a patient has gallstones, even after their removal they will most likely form again and become symptomatic. Thus, the most effective treatment method is surgery.
WHAT IS THE COST OF GALLBLADDER REMOVAL IN MEXICO?
$ 500.00 USD
If a patient chooses to have gallbladder removed at the time of their weight loss surgery (WLS), one fee of $500 USD will apply in addition to the bariatric surgery cost.
No additional lab work, medication, or hospitalization will be necessary, as WLS package has all such costs covered.
If you are interested in having gallbladder removal surgery as an independent procedure, please inquire with our patient coordinators about the cost.
WHAT ARE THE SIDE-EFFECTS OF LIVING WITHOUT A GALLBLADDER?
Some people develop diarrhea or more frequent softer stool after gallbladder removal. This side-effect is temporary and can last anywhere between several weeks to several months as the body adjusts to the consequences of the procedure.
Diarrhea after gallbladder removal seems to be related to the release of bile directly into the intestines. Normally, the gallbladder collects and concentrates bile, releasing it when you eat to aid the digestion of fat. When the gallbladder is removed, bile is less concentrated and drains more continuously into the intestines, where it can have a laxative effect. However, doctors found that the bile duct system eventually starts taking over some gallbladder functions. We are beautifully designed, and quite resilient.
Consider also that by the time you have gallbladder symptoms, you are already living without a gallbladder. If it is filled with multiple smaller stones or one large stone, it can no longer hold much bile, and you are living without your gallbladder`s proper function.
HOW CAN GALLSTONES BE PREVENTED?
Unfortunately, science doesn`t offer anything that could effectively prevent gallstones. Doctors report an increase of gallstones among younger people in the past 20 years, that goes along with the general trend to obesity and sedentary life style, as well as such health issues as diabetes and metabolic syndrome. Thus, any steps toward healthier life style that help our body in general, will help our gallbladder as much.
Common recommendations are:
• Adjusting your eating plan to include more foods high in fiber and healthy fats (such as olive oil, avocado oil, less animal fats), fewer refined carbohydrates, and less sugar.
• Losing weight safely if you are overweight or have obesity (unfortunately bariatric patients lose weight at a pace that is considered fast and will only increase chances to develop gallstones).
• Maintaining a healthy weight through healthy eating and regular physical activity.
STATISTICS
Society of American Gastrointestinal and Endoscopic Surgeons reports the rate of gallstone formation one year after RNY gastric bypass as high as 52.8%. (https://www.sages.org/meetings/annual-meeting/abstractsarchive/incidence-of-gallstones-after-sleeve-gastrectomy/) International Journal of Surgery (Volume 30, June 2016, Pages 13-18 (https://www.sciencedirect.com/journal/international-journal%20of-surgery) reports gallstone development after VSG (gastric sleeve) with the incidence of 47.9%. In addition, 47.8% of patients who developed gallstones became symptomatic. Majority of gallstones (95.8%) developed during the first 18 months after the surgery. Moreover, amount of weight loss and rate of weight loss were not significantly different between patients who developed gallstones and those who did not develop gallstones. Thus, everyone is at risk regardless of a lower or higher BMI.
